Negative Symptoms: Getting to the Specifics
Negative symptoms, a core symptom domain in schizophrenia, are described as a lessening or absence of normal behaviors and functions related to either motivation and interest, or emotional expression.
| Negative symptom dimensions | |
| Primary | Cause factor: schizophrenia, core symptom |
| Secondary | Cause factor: other symptoms of schizophrenia, depression, environment |
| Prominent | Intensity factor: more negative symptoms than positive symptoms |
| Predominant | Intensity factor: high level of negative symptoms, low positive symptoms |
| Persistent | Time factor: present for more than 6 months – 1 year |
References
- Mucci, A., Merlotti, E., Üçok, A., Aleman, A. & Galderisi, S. Primary and persistent negative symptoms: Concepts, assessments and neurobiological bases. Schizophr. Res. 186, 19–28 (2017).
- Carpenter, W. T., Heinrichs, D. W. & Alphs, L. D. Treatment of negative symptoms. Schizophr. Bull. 11, 440–452 (1985).
- Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 1: Update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J. Biol. Psychiatry 13, 318–378 (2012).
- Rabinowitz, J. et al. Negative symptoms in schizophrenia – the remarkable impact of inclusion definitions in clinical trials and their consequences. Schizophr. Res. 150, 334–338 (2013).
- European Medicines Agency. Guideline on clinical investigation of medicinal products, including depot preparation in the treatment of schizophrenia. (2012).
Markers of Inflammation and Infection in Schizophrenia
Molecular Psychiatry
Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis
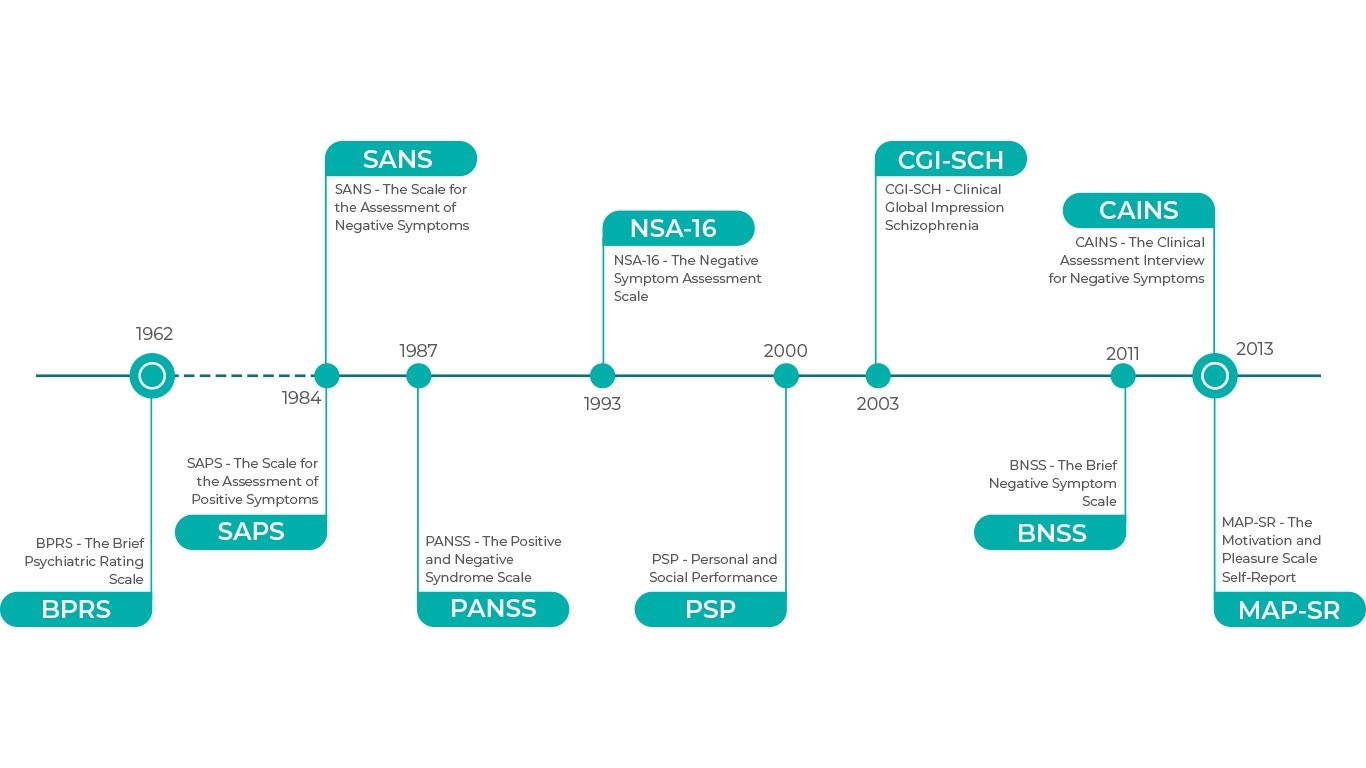
Selection of Schizophrenia Rating Scales
Rating scales help with monitoring the severity of symptoms in schizophrenia. Up until the 1980s, researchers focused on the positive symptoms, but later on they switched to both positive and negative symptoms.1
References
- Overall and Gorham. Psychological Reports. 1962;10:799-812
- Andreasen, University of Iowa, 1984
- Andreasen, University of Iowa, 1984
- Stanley et al. Schizophrenia Bulletin. 1987; 13(2):261–276
- Hopkins et al. Schizophrenia Bulletin. 2018; 44(3): 593–602
- Axelrod et al. Journal of Psychiatric Research. 1993; 27(3):253-258
- Morosini et al. Acta Psychiatr Scand. 2000;101(4):323-329
- Menezes et al. J Bras Psiquiatr. 2012;61(3):176-80
- Haro et al. Acta Psychiatr Scand Suppl. 2003;(416):16-23
- Kring et al. Am J Psychiatry. 2013;170:165–172
- Llerena et al. Compr Psychiatry. 2013;54(5): 568–574
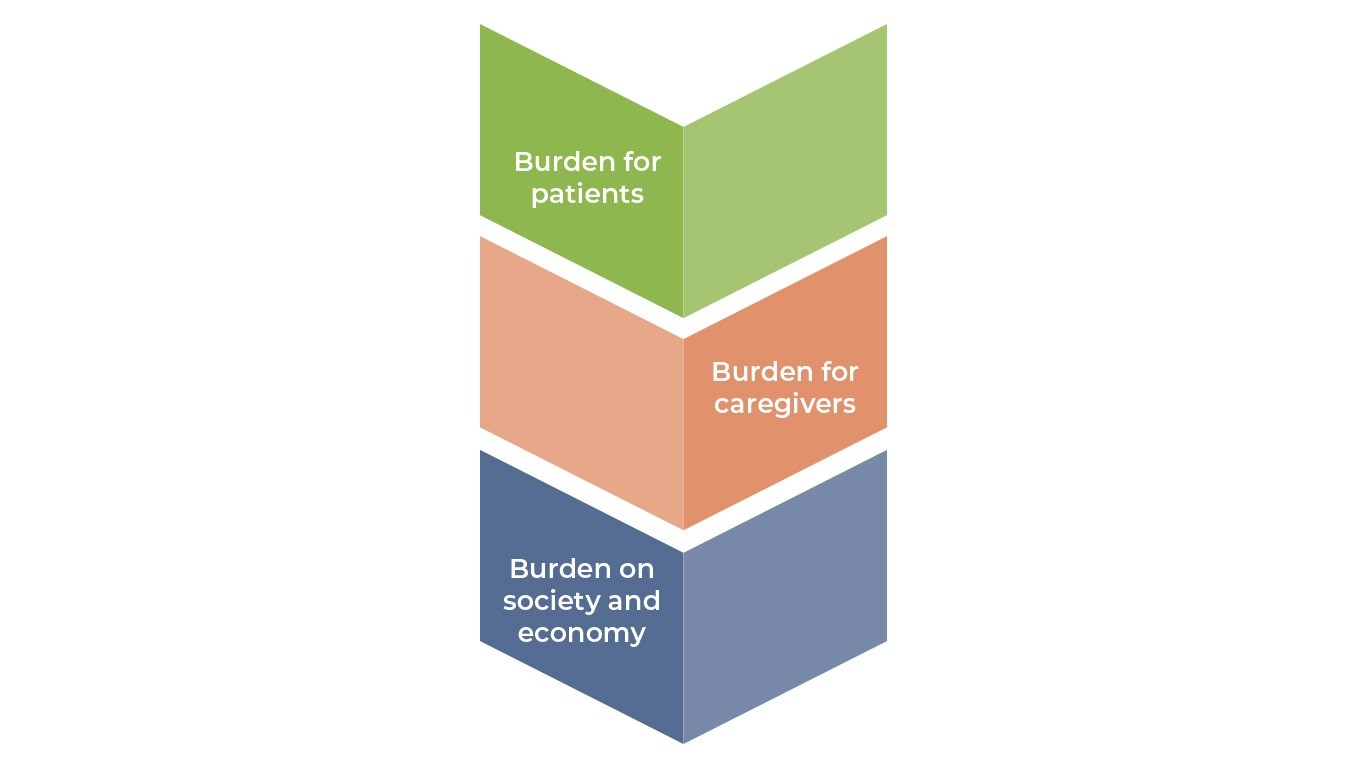
The Burden of Schizophrenia
Despite being a disorder with relatively low prevalence, schizophrenia is ranked among the top 25 leading causes of disability1. Even with best practice treatment, outcomes are often suboptimal given the complexity of the disorder and its wide-ranging consequences.
References
- Millier, A. et al. Humanistic burden in schizophrenia: A literature review. J. Psychiatr. Res. 54, 85–93 (2014).
- The National Alliance on Mental Illness. Schizophrenia: Public Attitudes, Personal Needs Views from People Living with Schizophrenia, Caregivers, and the General Public. (2008).
- Chong, H. Y. et al. Global economic burden of schizophrenia: A systematic review. Neuropsychiatr. Dis. Treat. 12, 357–373 (2016).
- Whiteford HA. Et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;9;382(9904):1575-86
DEVELOPMENT AND PSYCHOPATHOLOGY