Mastering the Diagnosis of Schizophrenia
- With no definitive blood test or brain scan available to detect schizophrenia, physicians must rely primarily on clinical symptoms to make a proper diagnosis, with special attention paid to symptoms that may suggest a differential diagnosis.
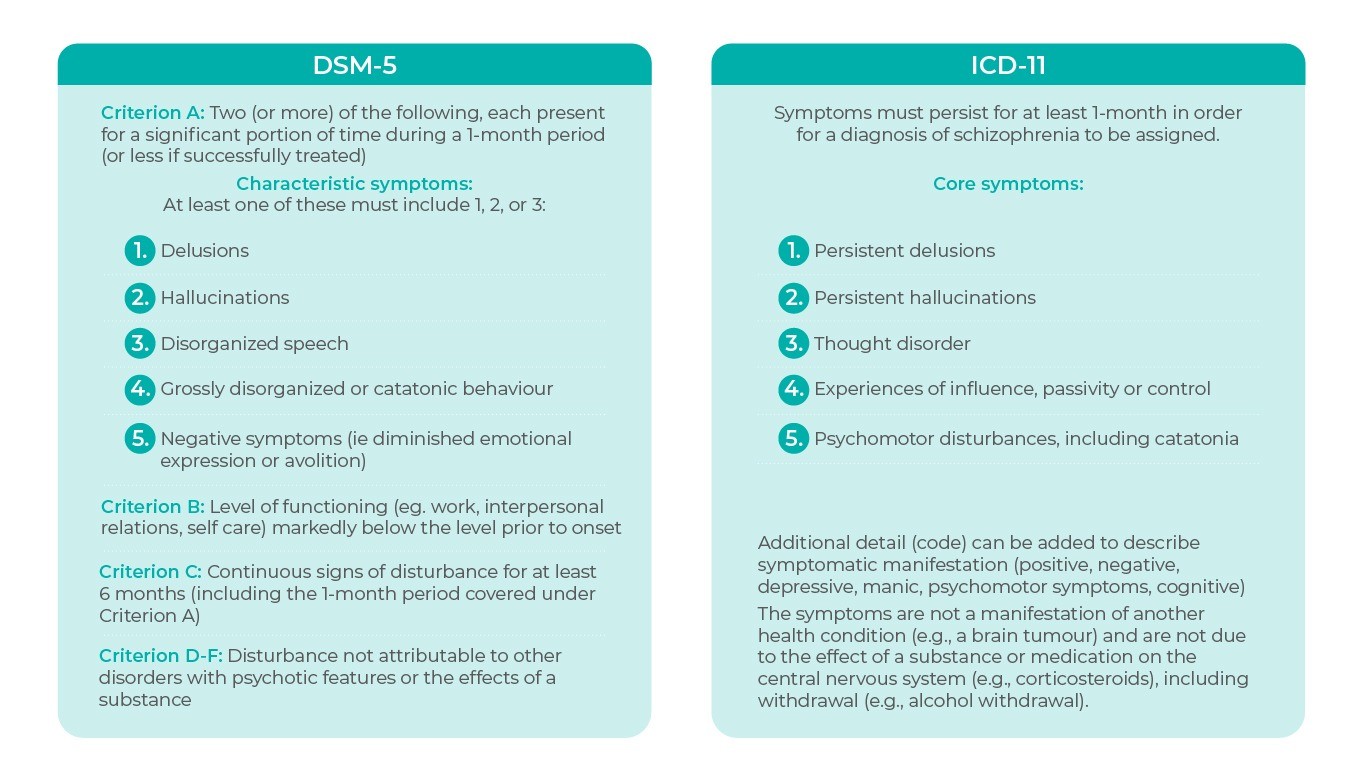
- Although they slightly differ, the International Classification of Diseases (ICD) and the Diagnostic and Statistical Manual of Mental Disorders (DSM) provide guidelines for the characterization and diagnosis of schizophrenia.
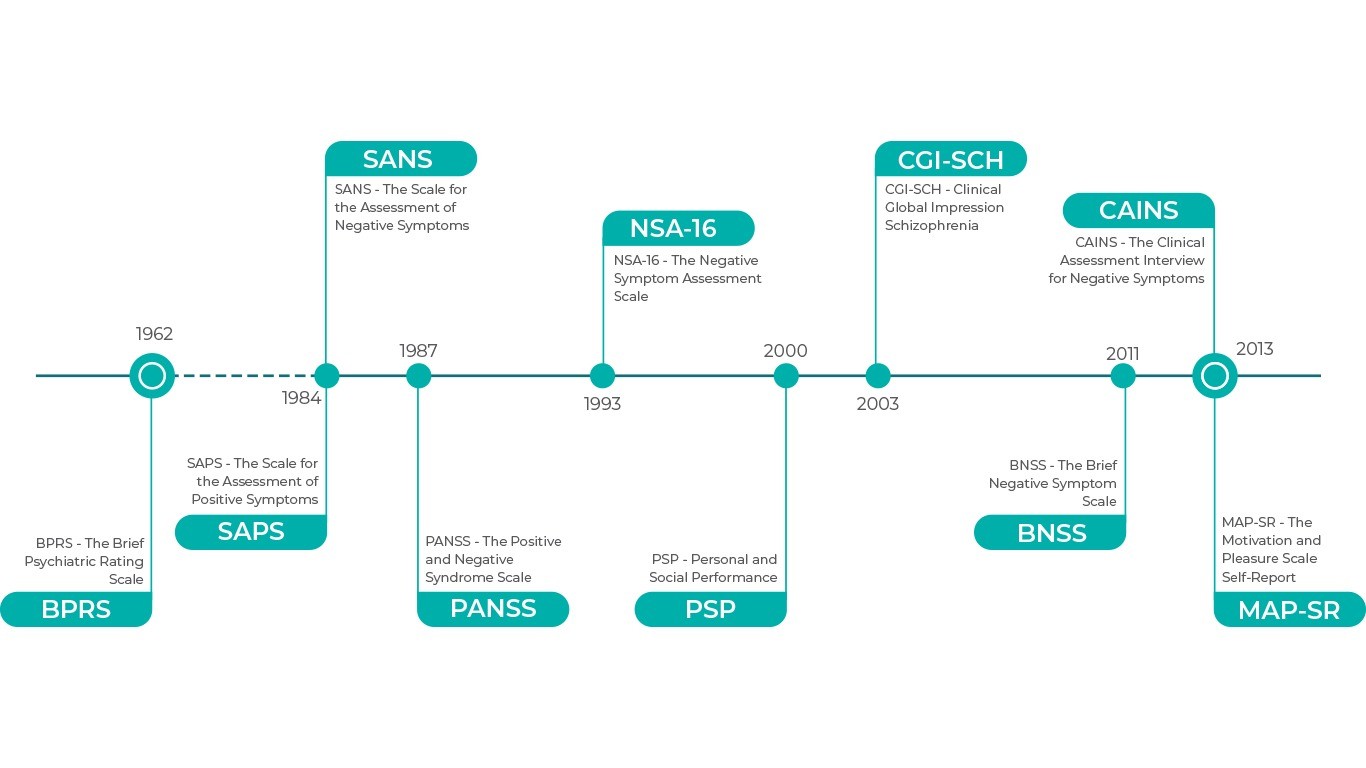
- Validated and well-established scales are available to evaluate positive and negative symptoms and to specify the severity of illness; newer scales have been specifically designed to evaluate negative symptoms.
In this section
No Blood Tests or Brain Scans…How Do you Diagnose?
Since no blood test or brain scan exists for schizophrenia, a great deal of attention must be paid to the constellation of symptoms that best define schizophrenia to ensure accurate diagnosis. The definition of schizophrenia has evolved through the views of Kraepelin (avolition, chronicity and poor outcome), Bleuler (fundamental symptoms [associative loosening, affective blunting, avolition, autism, ambivalence, attention] and accessory symptoms [hallucinations, delusions]) and Schneider (reality distortion/positive symptoms), with the relative importance of the various perspectives changing over time1. The development of the Diagnostic and Statistical Manual Of Mental Disorders (DSM) and World Health Organization International Classification of Disease (ICD) helped to define the essential features of schizophrenia, although the criteria used to diagnose the disorder continue to evolve. ICD and DSM criteria for schizophrenia differ slightly, but together they are routinely used to identify symptoms, diagnose the disorder, and codify it.
Diagnostic Criteria for Schizophrenia2,3
As can be expected in any classification system, the importance of some aspects of schizophrenia has been lost to the dimensional approaches of the DSM and ICD. For example, while positive symptoms are the predominant diagnostic feature of schizophrenia in both systems, negative symptoms alone are not sufficient to meet the criteria for a diagnosis of schizophrenia despite their impact on functioning and presence early in the course of illness (largely before an acute psychotic episode even leads to a diagnosis)4–6. Of additional concern, neurocognitive impairment, another core component of schizophrenia, is not mentioned as a diagnostic criterion in either classification system7. These observations should be considered as great limitations of the dimensional approach currently used to diagnose schizophrenia
Measuring the Symptoms of Schizophrenia: Clinical Scales
Clinical rating scales are used to evaluate symptoms and specify the severity of illness in schizophrenia. They can be viewed as a way to quantify clinical judgement of current psychopathology and change in symptoms over time. Most often used in clinical trials for evaluating the efficacy of schizophrenia treatments, scales are also used in clinical settings, although time constraints related to administration and the availability of trained raters are limiting aspects. Newer scales, with an eye toward convenience in the clinical setting and better assessment of negative symptoms, have been developed to evaluate schizophrenia, but there is no consensus regarding what rating scale is the best.
Rating Scales for Schizophrenia8-14
The Positive and Negative Syndrome Scale (PANSS)15 is the most frequently used clinical rating scale that was developed from the need to reduce the heterogeneity of what was known about schizophrenia. The PANSS has 30 items and 3 subscales; scores range from 1 (absent) to 7 (extreme), with higher scores indicating greater symptom severity. Items on the Positive Symptom subscale are delusions, conceptual disorganization, hallucinatory behavior, excitement, grandiosity, suspiciousness, and hostility. Negative symptom items (NS items) are blunted affect, emotional withdrawal, poor rapport, passive-apathetic social withdrawal, difficulty in abstract thinking, lack of spontaneity and flow of conversation, stereotyped thinking. Since stereotyped thinking and difficulty in abstract thinking are no longer considered negative symptoms, the inclusion of these items may confound the analysis of negative symptoms when the PANSS NS is used16. General psychopathology items, which are inconsistently related to either the positive or negative symptom domains, comprise somatic concern, anxiety, guilt feelings, tension, mannerisms and posturing, depression, motor retardation, uncooperativeness, unusual thought content, disorientation, poor attention, lack of judgment and insight, disturbance of volition, poor impulse control, preoccupation, active social avoidance.
Given the importance of negative symptoms as targets for drug development, newer scales have been developed for more accurate assessment of this domain. The Brief Negative Symptom Scale (BNSS)12 and the Clinical Assessment Interview for Negative Symptoms (CAINS)13 each have items that cover all 5 negative symptom constructs.
| Brief Negative Symptom Scale Items12 | Clinical Assessment Interview for Negative Symptoms Items13 |
| Anhedonia/avolition/asociality factor: • Anhedonia/intensity of pleasure • Anhedonia/frequency of pleasure • Anhedonia/intensity of expected pleasure • Distress • Asociality/behavior • Asociality/internal experience • Avolition/behavior • Avolition/internal experience | Motivation and pleasure factor: • Motivation for close family/spouse/partner relationships • Motivation for close friendships and romantic relationships • Frequency of pleasurable social relationships—past week • Frequency of expected pleasurable social relationships—next week • Motivation for work and school activities • Frequency of expected pleasurable work and school activities—next week • Motivation for recreational activities • Frequency of pleasurable recreational activities—past week • Frequency of pleasurable recreational activities—next week |
| Expressivity factor: • Blunted affect/facial expression • Blunted affect/vocal expression • Blunted affect/expressive gestures • Alogia/quantity of speech • Alogia/spontaneous elaboration | Emotional expressivity factor: • Blunted affect/facial expression • Blunted affect/vocal expression • Blunted affect/expressive gestures • Alogia/quantity of speech |
Differential Diagnosis: If not Schizophrenia, Then What?
Since the signs and symptoms of schizophrenia are not specific to schizophrenia alone, clinicians must first rule out other mental health or medical disorders that may present with psychotic symptoms, negative symptoms, or cognitive dysfunction before a diagnosis of schizophrenia can be made. This is accomplished through physical examination, medical history, tests and screening, psychiatric examination, the use of ICD criteria, and collaborative information obtained with permission from family and friends.
Diagnostic criteria for schizophrenia and other psychotic disorders reference 5 domains of psychopathology (hallucinations, delusions, disorganized speech, abnormal psychomotor behavior and negative symptoms). The severity and duration of symptoms from each of these domains can vary within individuals given the same diagnosis and can contribute to differential diagnostic decisions17.
Conditions to Rule Out: Differential Diagnoses for Schizophrenia3,18
| Differential Diagnoses | Why It’s Not Schizophrenia according to ICD-11 |
| Schizoaffective disorder (6A21) | Prominent mood component; Diagnostic requirements of schizophrenia and of manic, mixed, or moderate or severe depressive episode are met within the same episode of illness |
| Schizotypal disorder (6A22) | Long-standing (≥ 2 years) pattern of odd beliefs and/or perceptual disturbances that do not rise to the level of delusions or hallucinations |
| Acute and transient psychotic disorder (6A23) | Acute onset of psychotic symptoms that emerge without a prodrome and reach their maximal severity within 2 weeks; does not exceed 3 months, and most commonly lasts from a few days to 1 month |
| Delusional disorder (6A24) | Delusions only, without other symptoms of schizophrenia (e.g. persistent auditory hallucinations, disorganized thinking, negative symptoms); persist for at least 3 months |
| Schizophreniform disorder (ICD-10, F23.2)* | Total duration of the disorder is less than 1 month |
| Schizoid personality disorder (ICD-10, F60.1)* | Long-standing pattern of little interest in social relationships or intimacy; overlap with the negative symptoms, disorder does not present with psychosis |
| Substance abuse or substance-induced psychosis (6C) | Symptoms are a manifestation of intoxication or acute withdrawal, and are in close temporal relationship with consume or withdrawal |
| Bipolar mania with psychotic symptoms (6A60) | Prominent mood component; psychosis only occurs in the presence of a mood episode and does not rise to the level of schizophrenia |
| Bipolar depression (6A60) or major depressive disorder (with psychotic or catatonic features) (6A70) | Prominent mood component; psychosis only occurs in the presence of a mood episode and does not rise to the level of schizophrenia |
| Posttraumatic stress disorder, Body dysmorphic disorder, Obsessive-compulsive disorder | Rarely also accompanied by psychotic symptoms |
| Neurology: CNS tumors, temporal lobe epilepsy, frontal or limbic trauma, cerebrovascular events, Huntington’s disease, metachromatic leukodystrophy, hydrocephalus, Wernicke-Korsakoff syndrome, Wilson’s disease, Jacob-Creutzfeldt’s disease | Symptoms are due to other medical condition |
| Infections: AIDS, Syphilis, Herpes encephalitis | Symptoms are due to other medical condition |
| Endocrine disorders | Symptoms are due to other medical condition |
| Metabolic events (acute intermittent porphyria, Vit B12 deficiency, carbon monoxide poisoning, homocystinuria, heavy metal poisoning) | Symptoms are due to other medical condition |
| Fabry’s disease, Fahr’s disease, Hallervorden-Spatz disease, Systemic Lupus erythematosus, Anti-NMDA receptor encephalitis | Symptoms are due to other medical condition |
*Not specified in ICD-11 any more
References
- Tandon, R. et al. Definition and description of schizophrenia in the DSM-5. Schizophr. Res. 150, 3–10 (2013).
- American Psychiatric Association. DSM-5 Diagnostic Classification. in Diagnostic and Statistical Manual of Mental Disorders (2013). doi:10.1176/appi.books.9780890425596.x00diagnosticclassification
- WHO. International statistical classification of diseases and related health problems – 10th revision. World Heal. Organ. (2011).
- Tarbox, S. I. & Pogue-Geile, M. F. Development of Social Functioning in Preschizophrenia Children and Adolescents: A Systematic Review. Psychol. Bull. 134, 561–583 (2008).
- Matheson, S. L. et al. Systematic meta-analysis of childhood social withdrawal in schizophrenia, and comparison with data from at-risk children aged 9-14 years. J. Psychiatr. Res. 47, 1061–1068 (2013).
- Schmidt, A. et al. Improving Prognostic Accuracy in Subjects at Clinical High Risk for Psychosis: Systematic Review of Predictive Models and Meta-analytical Sequential Testing Simulation. Schizophr. Bull. 43, 375–388 (2017).
- Keefe, R. S. E. Should cognitive impairment be included in the diagnostic criteria for schizophrenia? World Psychiatry 7, 22–28 (2008).
- Overall, J. E. & Gorham, D. R. The Brief Psychiatric Rating Scale. Psychol. Rep. 10, 799–812 (1962).
- Andreasen, N. C. Scale for the Assessment of Positive Symptoms (SAPS). Br. J. Psychiatry. Suppl. (1984).
- Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
- Axelrod, B. N., Goldman, R. S. & Alphs, L. D. Validation of the 16-item negative symptom assessment. J. Psychiatr. Res. 27, 253–258 (1993).
- Kirkpatrick, B. et al. The brief negative symptom scale: Psychometric properties. Schizophr. Bull. 37, 300–305 (2011).
- Kring, A. M., Gur, R. E., Blanchard, J. J., Horan, W. P. & Reise, S. P. The Clinical Assessment Interview for Negative Symptoms (CAINS): Final development and validation. Am. J. Psychiatry 170, 165–172 (2013).
- Llerena, K. et al. The Motivation and Pleasure Scale-Self-Report (MAP-SR): Reliability and validity of a self-report measure of negative symptoms. Compr. Psychiatry 54, 568–574 (2013).
- Kay, S. R., Opler, L. & Fiszbein, A. Positive and Negative Syndrome Scale Manual. (North Tonawanda, N.Y.: Multi-Health systems, 2000).
- Daniel, D. G. Issues in Selection of Instruments to Measure Negative Symptoms. Schizophr. Res. 150, 343–345 (2013).
- Barch, D. M. et al. Logic and justification for dimensional assessment of symptoms and related clinical phenomena in psychosis: Relevance to DSM-5. Schizophr. Res. 150, 15–20 (2013).
- Fatemi, S. H. & Clayton, P. J. The medical basis of psychiatry: Fourth edition. The Medical Basis of Psychiatry: Fourth Edition (2016). doi:10.1007/978-1-4939-2528-5
Annual Review of Clinical Psychology
Psychiatric Diagnosis: Lessons from the DSM-IV past and cautions for the DSM-5 future.

ICD and DSM criteria for schizophrenia differ slightly, but together they are routinely used to identify symptoms of schizophrenia, diagnose and codify it.
Download