Quick Overview: What is Schizophrenia?
- Schizophrenia, a complex neuropsychiatric syndrome, is a chronic mental illness that generally requires continual treatment to prevent relapse and recurrence.
- Schizophrenia is commonly considered a neurodevelopmental disorder; however, unlike some other disorders of this kind, the symptoms of schizophrenia often do not become apparent for decades.
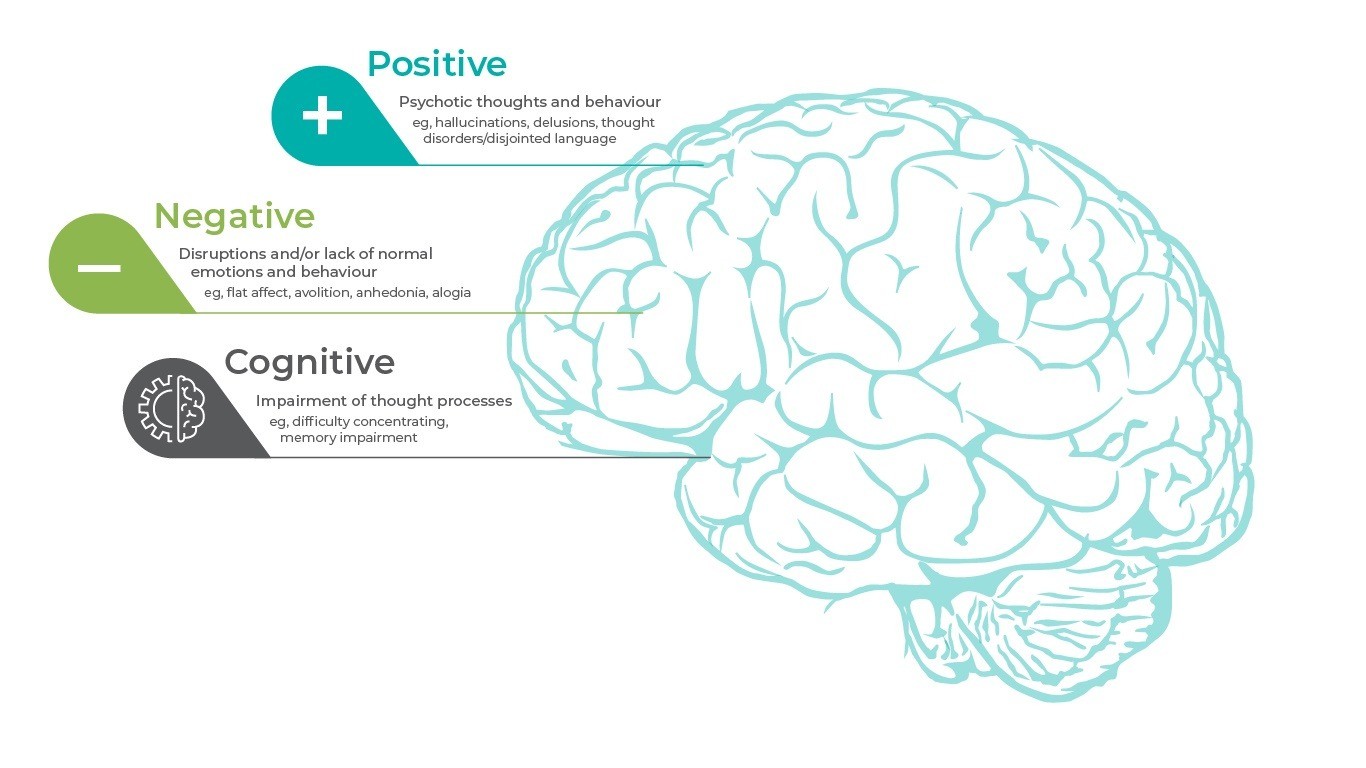
- Schizophrenia is heterogeneous, with no single pathognomonic symptom or presentation; the constellation of signs and symptoms associated with schizophrenia are divided into 3 core symptom domains: positive, negative, and cognitive.
In this section
A Biological Basis for Schizophrenia
Neuropsychiatric syndromes, such as schizophrenia, have symptoms that affect brain function, emotion, and mood. Although the specific cause of schizophrenia is unknown, it has a biologic basis as seen by alterations in brain structure (eg, enlarged cerebral ventricles, thinning of the cortex, decreased size of the anterior hippocampus and other brain regions), changes in neurochemistry (eg, altered activity in dopamine, serotonin, and glutamate transmission markers), and demonstrated genetic risk factors1.
| Neurotransmitter | Effect in schizophrenia |
| Dopamine | Mediates positive and negative symptoms |
| Serotonin | Mediates mood symptoms |
| Glutamate | Mediates positive and negative symptoms |
The heritability of schizophrenia is approximately 80%, but it is thought that there are multiple susceptibility genes, each having a small effect along with influential epigenetic and environmental factors2.
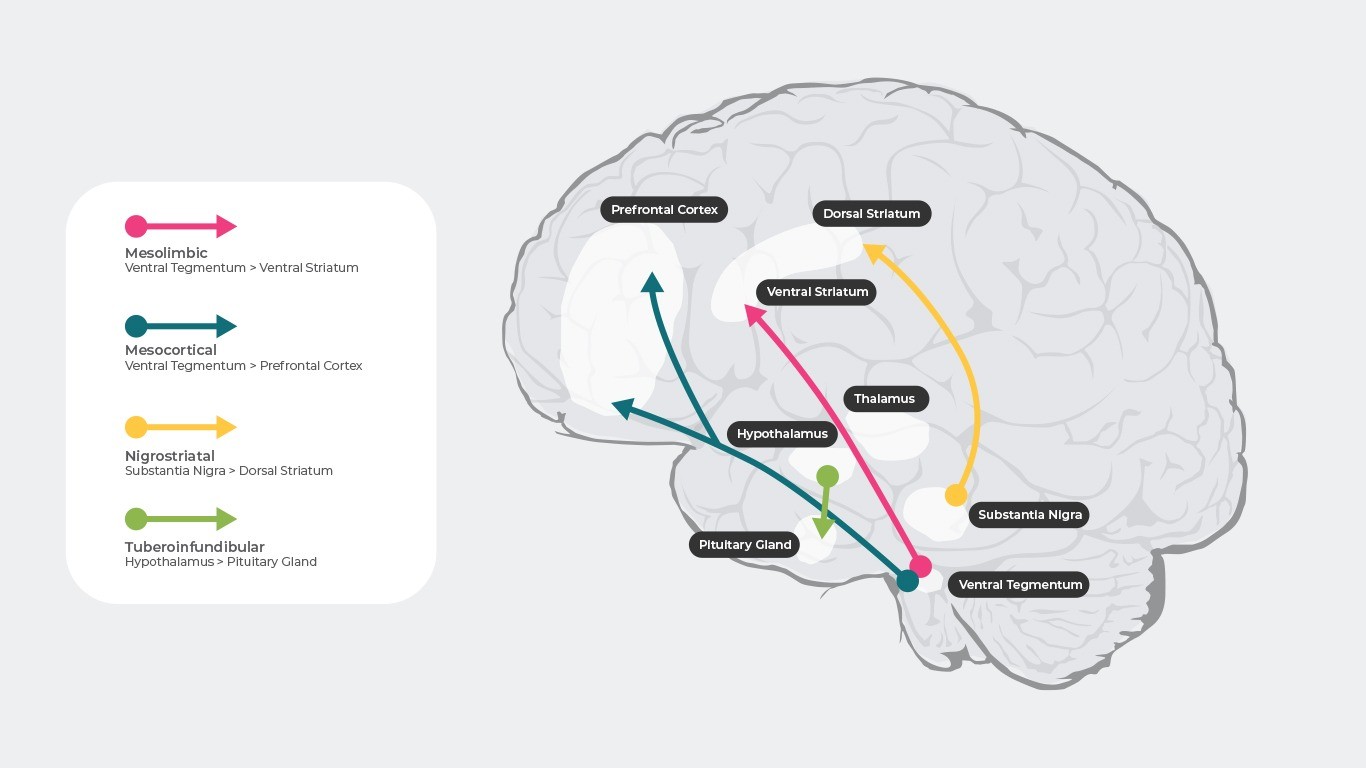
Dopaminergic Pathways Associated With Schizophrenia
The neurotransmitter dopamine controls many different functions in the brain including cognition, emotion, positive reinforcement, and hormone regulation3. There are 4 main dopamine pathways that are thought to be involved in schizophrenia4.
Positive symptoms of schizophrenia are thought to arise due to the hyperactivity of dopamine in the mesolimbic pathway. This proposed dysfunction is sometimes referred to as the „dopamine theory of schizophrenia”4–6.
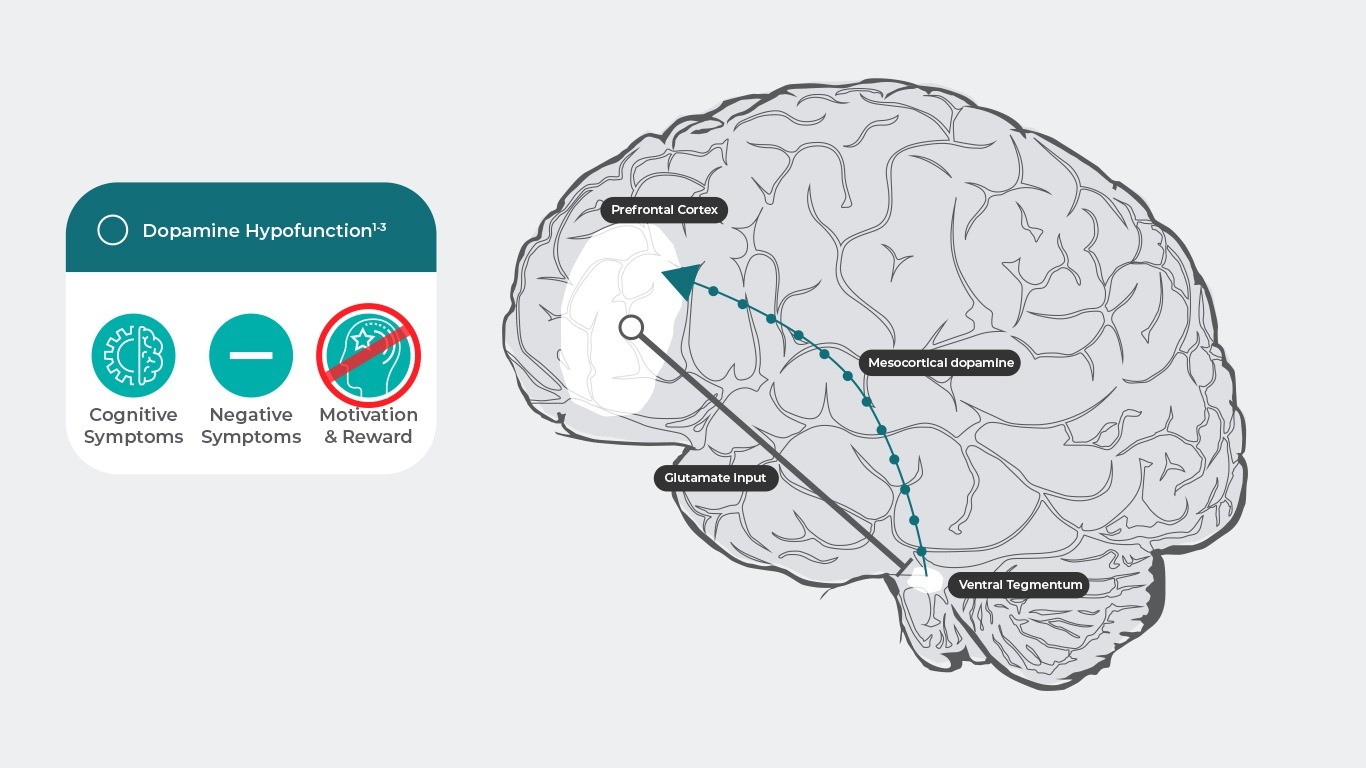
Negative symptoms of schizophrenia are thought to arise due to a hypoactivity of dopamine in the mesocortical pathway4–6.
Neurodevelopmental Vulnerabilities
Schizophrenia may occur more frequently in people with neurodevelopmental vulnerabilities; the onset, remission, and recurrence of symptoms are thought to be the result of interactions between these enduring vulnerabilities and environmental stressors. Schizophrenia rarely presents in early childhood, but prenatal and early childhood factors such as genetic predisposition, birth complications, central nervous system infections, and trauma and neglect influence disease onset in adulthood1,7,8.
Three Core Symptom Domains
Although symptom combinations and patterns vary considerably among patients with schizophrenia and change over time in individuals, there are 3 core symptom domains: positive, negative, and cognitive1.
The clinical diagnosis of schizophrenia relies heavily on the positive symptoms associated with a prolonged psychotic episode. Positive symptoms are classically defined as an excess or distortion of normal functions1:
Delusions are fixed beliefs that are not changeable even in light of conflicting evidence; they occur in approximately 80% of people with schizophrenia9.


Hallucinations are perceptual experiences that occur without external stimuli; auditory hallucination are the most common kind, occurring in between 40%-80% of people with schizophrenia9, 10.


Negative symptoms are considered a reduction or absence of normal function related to motivation and expression; they occur independently of positive symptoms, cognitive dysfunctions, disorganization, and depression11. Negative symptoms are either primary to the underlying schizophrenia pathology or secondary to other factors (eg, positive, affective, or extrapyramidal symptoms, antipsychotic side effects, sedation, environmental deprivation, illness- or treatment-related factors11,12.


Cognitive symptoms affect a complex collection of mental processes including perception, learning, thinking, memorizing, analyzing, and adaptive behaviors. Cognitive impairment is considered one of the most disabling dimensions of schizophrenia and in many cases, it persists during pharmacological treatment13.


The severity, duration, and frequency of the clinically heterogeneous symptoms of schizophrenia vary among patients and change over time. Frequently chronic and debilitating, the risk-benefit ratio favors continuing long-term antipsychotic treatment for patients with schizophrenia since evidence shows that antipsychotics are effective against positive symptoms and reduce the risk of relapse. Studies suggest that discontinuing antipsychotic treatment results in relapse for up to 75% of patients within 12 to 18 months14-16.
References
- Tamminga, C. A. Schizophrenia. Merck Manual Professional Version (2018). Available at: https://www.merckmanuals.com/professional/psychiatric-disorders/schizophrenia-and-related-disorders/schizophrenia#v39692526.
- Tamminga, C. A. & Holcomb, H. H. Phenotype of schizophrenia: A review and formulation. Molecular Psychiatry (2005). doi:10.1038/sj.mp.4001563
- Missale, C., Fiorentini, C., Collo, G. & Spano, P. The neurobiology of dopamine receptors: Evolution from the dual concept to heterodimer complexes. J. Recept. Signal Transduct. 30, 347–354 (2010).
- Stahl, S. M. Stahl ’ s Essential Psychopharmacology: Neuroscientific Basis and Practical Applications. (2013).
- Howes, O., McCutcheon, R. & Stone, J. Glutamate and dopamine in schizophrenia: An update for the 21st century. J. Psychopharmacol. 29, 97–115 (2015).
- Elert, E. Aetiology: Searching for schizophrenia’s roots. Nature 508, S2-3 (2014).
- Working Group of the Psychiatric Genomics Consortium, S. Biological insights from 108 schizophrenia-associated genetic loci. Nature 511, 421–427 (2014).
- Khandaker, G. M. et al. Inflammation and immunity in schizophrenia: Implications for pathophysiology and treatment. The Lancet Psychiatry 2, 258–270 (2015).
- Andreasen, N. C. Schizophrenia: the characteristic symptoms. Schizophr. Bull. 17, 27–49 (1991).
- Thomas, P. et al. Correlates of hallucinations in schizophrenia: A cross-cultural evaluation. Schizophr. Res. 92, 41–49 (2007).
- Galderisi, S., Mucci, A., Buchanan, R. W. & Arango, C. Negative symptoms of schizophrenia: new developments and unanswered research questions. The Lancet Psychiatry 5, 664–677 (2018).
- Carpenter, W. T., Heinrichs, D. W. & Alphs, L. D. Treatment of negative symptoms. Schizophr. Bull. 11, 440–452 (1985).
- Green, M. F. Impact of cognitive and social cognitive impairment on functional outcomes in patients with schizophrenia. J. Clin. Psychiatry 77, 8–11 (2016).
- Correll, C. U., Rubio, J. M. & Kane, J. M. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry 17, 149–160 (2018).
- Davis, J. M., Metalon, L., Watanabe, M. D. & Blake, L. Depot Antipsychotic Drugs: Place in Therapy. Drugs 47, 741–773 (1994).
- Kissling, W. The current unsatisfactory state of relapse prevention in schizophrenic psychoses – Suggestions for improvement. Clin. Neuropharmacol. 14, S33-44 (1991).
Molecular Psychiatry
Phenotype of schizophrenia: a review and formulation.
There are 4 main dopamine pathways in the brain. The mesocortical and mesolimbic are disturbed in schizophrenia.
DownloadReferences title